Orthodontic Practice US, September 23, 2019
Editor’s intro: Preventing orthodontic relapse is tricky — caused by both clinical reasons and patient non-compliance, but orthodontists have some choices on keeping their patients’ beautiful smiles intact.
Dr. Ricky E. Harrell examines reasons for relapse following completion of active orthodontic treatment.
Background
Retention — the 800 lb. gorilla in the orthodontic room. If you want opinions on retention, ask 10 orthodontists, and you will probably hear several differing views on effective retention protocol.
Orthodontic relapse and posttreatment problems have existed since the first active appliance therapy on a patient was discontinued, and the patient’s active treatment was considered competed. The realization of the difficulties of retention dates back to the words of the most universal name in orthodontic retention, Dr. Charles Augustus Hawley. In an essay presented on March 1919 to the Eastern Association of the Graduates of the Angle School of Orthodontics in Baltimore, Maryland, Dr. Hawley was attributed with passing along two statements of his contemporaries with regards to the retention process.
The first statement was from his colleague, who stated, “Any fool can move teeth, but it takes a wise man to make them stay.” Another quote attributable to Dr. Hawley’s colleagues was, “If anyone would take my cases after they are finished, retain them, and be responsible for them afterward, I would give him half the fee.”1 For the most part, these words still ring true in contemporary orthodontic practice, regardless of the method used to align the dentition and establish the occlusion.
In an article published by Dr. George Hahn in 1944 entitled “Retention — The Stepchild of Orthodontia,” he stated, “The newer concept of retention was evolved the hard way, that is by clinical evidence, the result of trial and error, and in all clinical evidence in the history of orthodontia, this one basic fact stands out: That irrespective of the length of time a tooth is held in its new position by any means whatsoever, it will upon release seek a position where it is in balance with the forces that act upon the denture; whether these forces are for good or evil is immaterial, the greatest of these forces is the force of occlusion.”2
Dr. Hahn went on in the article to list some of what he felt were causes of relapse, many of which are pertinent today, especially in the era of non-extraction-at-all-costs treatment. Among those listed were the following that are especially applicable in today’s era:
The problem of retention and stability in orthodontics is well over a century-old. In this article we will examine reasons for relapse and emphasize one that is almost universal and yet receives little attention.
Stretching of the periodontal ligament fibers
First reported in studies done on dogs by Reitan, it was noted via biopsy, tissue staining, and light microscopy that fibers in the periodontal ligament were stretched during orthodontic rotational movement. Fibers in the apical third of the root were stretched less than fibers in the middle third and even less than fibers in the gingival or the “marginal” third of the root due to the differing circumferences of the root area as one progresses toward the apex from the marginal area. At 232 days of retention, the biopsies demonstrated that the apical- and middle-third fibers had reorganized well, but that the marginal fibers were only partly re-organized at that point in time.3
It was also noted that at the 232-day mark of retention, new bone was well organized along the stretched periodontal ligament fibers in both the apical and middle third of the roots but only fairly organized along the stretched fibers in the marginal third of the root.3
Redlich, in another relapse study using dogs as the experimental models in 1996, utilized scanning electron microscopy (SEM) as well as transition electron microscopy (TEM) to observe microscopic changes in the periodontal ligament as well as connective tissue fibers in the lamina propria of the gingival tissues around the tooth. Redlich noted that the whole gingival apparatus seemed to move with the rotational movement of the tooth and postulated that the supra-alveolar fibers were not stretched but maintained their continuity with the lamina propria as the whole gingival apparatus was moving with the tooth, and that the elasticity in the gingival tissue, as evidenced by an increase in oxytalan fibers, was partially responsible for relapse.4
The relationship of alveolar bone to orthodontic relapse was investigated by Sharpe, et al., in 1987. Using lateral cephalometric radiographs, bitewings, and full-mouth radiographic series on patients at least 10 years out of retention, it was noted that the greatest amount of relapse occurred in patients who had the greatest amount of tooth movement and the greatest translational movement of teeth, and experienced the greatest amount of root resorption. Crestal alveolar bone was also diminished in the group demonstrating the greatest amount of relapse.5
The thickness of alveolar cortical bone in the incisor region has also demonstrated a positive relationship to orthodontic stability. Rothe, et al., demonstrated that patients with thinner mandibular cortical bone — i.e., long, teardrop-shaped symphysis — exhibit a greater tendency for orthodontic relapse in comparison to patients with a greater thickness of alveolar bone.6 One can extrapolate thickness of cortical bone in the mandibular symphysis to the facial skeletal type — i.e., a brachycephalic patient with a thick, short symphysis would demonstrate thicker cortical bone than would a dolichocephalic patient with a long, narrow, teardrop-shaped symphysis (Figures 1 and 2).
Posttreatment mandibular rotation, especially in a counterclockwise pattern, has been discussed as a potential source of incisor relapse due to deepening of the bite over time or prolonged mandibular growth in Class III patients. Research generally points to a very nominal or no role in incisor relapse following treatment.
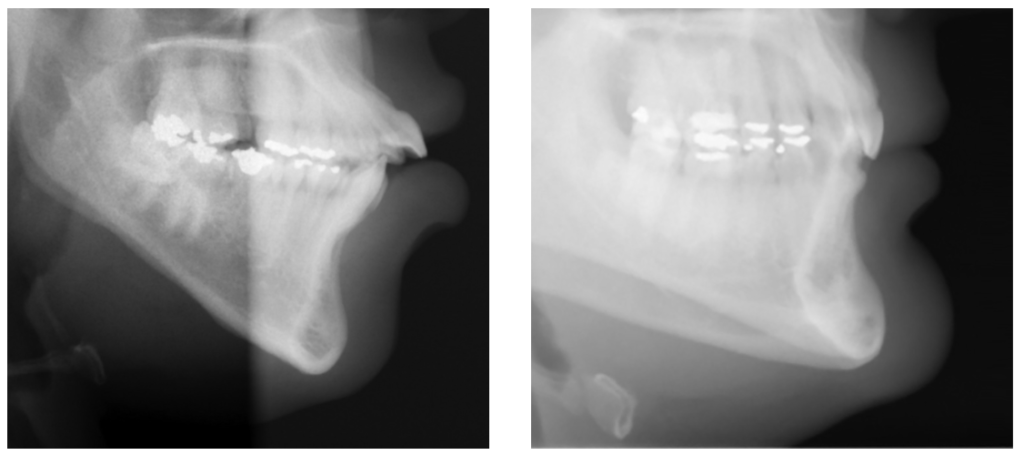
Figure 1: Dolichocephalic patient — thin cortical bone (left) and Figure 2: Brachycephalic patient — thick cortical bone (right)
In the 1950s, Straub generated a wave of excitement among orthodontists with the observations that tongue thrusting was a major component of the creation of an anterior open bite, and that vertical relapse of the incisors could be attributed to tongue thrusting. It seemed logical that patients who swallowed incorrectly should have protruding incisors either before treatment or could relapse to that condition, but after studies were done, it became apparent that tongue and lip pressures during swallowing varied greatly among individuals and did not correlate well with position of the teeth.7
Whalen later demonstrated that vertical pressure on the incisors by the tongue during swallowing has little to do with vertical positioning of anterior teeth. His study demonstrated that vertically directed tongue pressures during swallowing in patients with anterior open bites are less that those with normal vertical relationships.8
In 1975, Proffitt and Mason summed up the phenomena of soft tissue effects, especially with the tongue, when they stated that the resting posture/position of the tongue and its subsequent pressure on the dentition has a much greater influence on tooth position than does pressure by the tongue during swallowing. They also felt that in an effort to reduce orthodontic relapse in patients that actually did exhibit tongue thrust and anterior tongue posture at rest, myofunctional therapy during orthodontic treatment was most effective as opposed to therapy that is done prior to orthodontic treatment.9 It has also been demonstrated that oromyofunctional therapy done in conjunction with orthodontic therapy is more effective in maintaining open bite correction than is orthodontic therapy alone.10
What role might lip pressure play in orthodontic relapse? It is generally agreed that lip pressure exerted on the teeth is less than tongue pressure, and that there is not a balance between pressure exerted on the dentition by the tongue and lips. Again, posture of the lip, especially lower lip, plays a role in relapse. Interposed lower lips and lip pressure can contribute significantly to orthodontic relapse of maxillary incisors.11 However, Doto and Yamato found that pressure exerted by the lips is more contributory to proclined incisor position in Class II patients than is tongue pressure.12 Regardless of whether the tongue or lips is most influential on relapse after orthodontic therapy, the role of both must be considered and that teeth should be placed in what is the most harmonious relationship with the soft tissue envelope as determined by the practitioner, and that resting tongue posture be normalized as much as is possible (Figures 3-5).

Figure 3: Patient at age 11.2 — pretreatment (left), Figure 4: Patient at age 15.2 — day of appliance removal (middle), and Figure 5: Patient at age 17.5 — 2-year post-debonding with tongue habit still active (right)
Persistence of digit habits such as thumb- or finger-sucking has been recognized as a factor in orthodontic relapse. Successful dental open bite correction may be negated with orthodontic vertical anterior relapse if digit habits persist following orthodontic therapy.13,14 The incidence, duration, and intensity of the habit will determine if the teeth will compensate unfavorably for the habit following treatment.
With the introduction of self-ligating appliances back into the orthodontic marketplace some 20 years ago, the principles of orthodontic stability have taken a back seat to the pursuit of non-extraction orthodontic approaches. Although as a profession we have decreased percentages of extraction treatment to orthodontic treatment as a whole, some have felt that moderation in choosing extraction therapy was not enough, and that non-extraction therapy should be pursued at all cost. How might this contribute to relapse?
Inherent to non-extraction treatment in crowding cases where the crowding exceeds 7 mm-8 mm in the mandibular arch is the resultant proclination of mandibular incisors (Figures 6-8) and resultant increase in arch length as well as a deviation from the original mandibular arch form (Figures 9 and 10). Another unintended consequence of non-extraction therapy at all costs is the expansion of mandibular canines greater than 1 mm-1.5 mm in treatment, which in most cases is doomed to eventual relapse.15,16,17,18,19
Does the literature support the concept that increasing arch length during treatment is doomed to relapse? Yes, it does and has so for many years. In my opinion, one of our outstanding orthodontic practitioners, Dr. James Boley, summed up this concept up in a presentation entitled “Why Try to Fit Teeth into an Ever-Shrinking Arch?” given in the early 1980s to the Colorado Orthodontic Society. An increase in proclination of mandibular incisors, if the mandibular molars do not move mesially, arbitrarily increases mandibular arch length. Study after study demonstrates that this is unstable over the course of a lifetime after retention is discontinued.20,21,22,23,24,25
Relapse tendency is also heightened if there is a significant deviation in arch form from the existing mandibular arch. Again, this is well documented in the literature.26,27,28,29 If mandibular arch form is either willingly or unwillingly violated during treatment, relapse is almost certain after discontinuance of retention.
Expansion of the mandibular canines, with rare exception due to canines lingually positioned in the original malocclusion, is also a contributor to orthodontic relapse. Again, this is more than adequately documented and, despite this, some currently willingly and routinely violate this principle with non-extraction modalities.
The quality of the result of treatment, as judged by occlusal fit, did not seem to be influential in relapse with as much relapse tendency noted in “well-treated” cases as in cases with less desirable outcomes.30,31
Thus far, we have discussed a number of factors in the physical realm of tooth movement that contribute to relapse. Is there something about relapse outside of the realm of tooth movement, anatomic limitations, and physiologic phenomena, which influence relapse, that we have not discussed? Indeed, there is, and that factor is patient cooperation with retention.
In our inspection of patient cooperation as a cause of relapse, there is some solace to be found with our brothers and sisters in medicine. Just so that we don’t feel alone in our endeavors with retainer wear, in the medical literature on patient behavior, it was found that less than one-third of asthma patients ever comply with medication instructions, regardless of whether they were educated about the benefits of taking the medication or not, regardless of the severity of the disease or condition to be treated.32
In a study by Kacer, et al., it was found that based on the minimal standard of nighttime retainer wear at the 3-month post-debond mark, fully 31% of patients were not cooperative. At the 7-9 month mark, that percentage had increased to 45% of noncooperation, and at the 19-24 month mark, the percentage of patient cooperating with night-only retainer wear had increased to 55%, and cooperation, as judged by regular nighttime wear, had diminished to 45%.33
Another question to be asked about cooperation with retainers is, Does the type of retainer make a difference with retention? Obviously, fixed retention eliminates one set of cooperation variables but introduces its own set of problems outside of cooperation. What about Hawley-type retainer versus vacuum-formed Essix-type retainers?
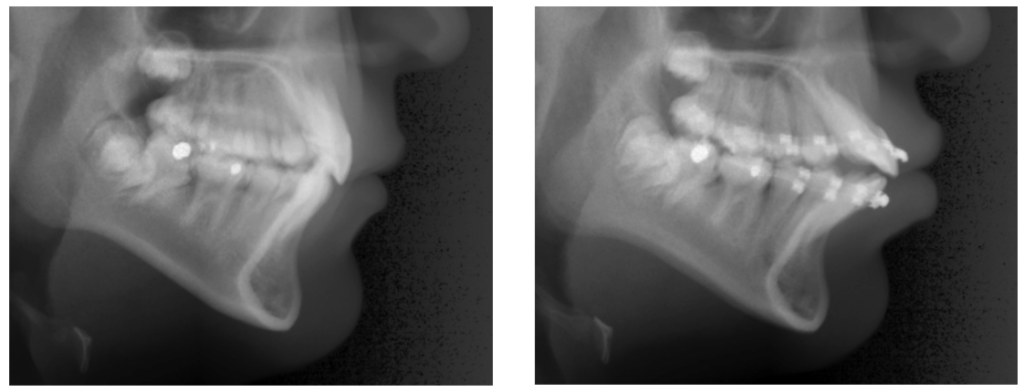
Figure 6: Incisor position prior to appliance placement (left) and Figure 7: Arch length increase and incisor proclination as a result of non-extraction approach (right)
In a study done at the University of Kentucky, it was found that patients were more likely to be cooperative with Essix-type retainers early in retention but more likely to be cooperative with Hawley-type retainers as the retention time from debonding increased. The study determined that among the variables that influenced cooperation were the patient’s understanding of the importance of retainer wear (patient education), the amount of time since debonding (patient fatigue), the patient’s age (older patients less compliant than younger patients), patient’s gender (males less cooperative than females), and type of retainer provided.34

Figure 8: Resultant bone loss, instability due to excessive proclination
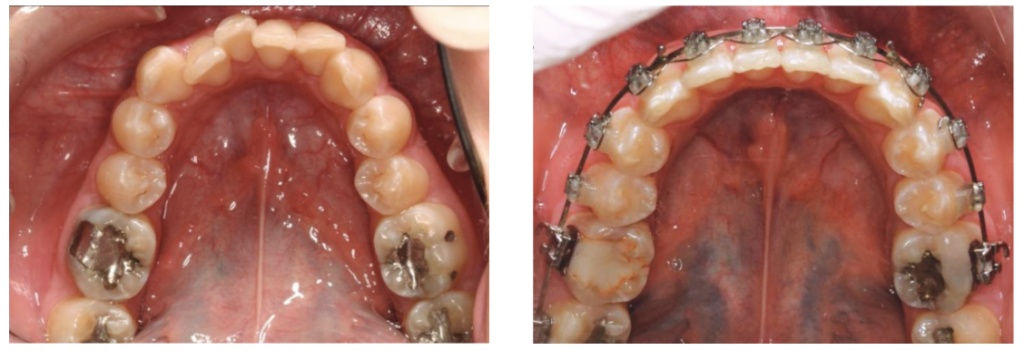
Figure 9: Pretreatment arch form (left) and Figure 10: Change in mandibular arch form as a result of appliance therapy (right)
Based on the evidence presented, the following suggestions are made to minimize the negative effects of relapse following the active treatment stage.
Despite extensive research, the various elements leading to relapse of treated mal-occlusions are incompletely understood, giving rise to wide variation in retention protocols among clinicians. Informed consent — with emphasis on the features of the original malocclusion and the patient’s growth pattern, the type of treatment performed, the need for adjunctive surgical procedures, the type of retainer, and the duration of retention — should be obtained during the treatment-planning stage. True perspective on orthodontic retention is lacking, and there is a great need for further research to ensure that evidence-based clinical practice is adopted in retention strategies.35
Orthodontic relapse continues to be a significant issue that we all, as clinicians, must manage. By following the suggested guidelines, relapse can be minimized and manageable within the practice. Stability is one of the most important aspects of treatment to patients. We should strive to provide that for all of our patients and continually work to improve our outcomes.
Dr. James Bonham offers some of his insights into orthodontic relapse in “Retention — esthetics, delivery, and long-term success”.
Author Info
Ricky E. Harrell, DMD, MA, is a 1979 graduate of the University of the Alabama School of Dentistry. After serving as a Commissioned Officer in the U.S. Public Health Service in the Navajo Area Indian Health Service for 3 years, he returned to the University of Alabama and completed his residency in orthodontics in 1984. He was in the private practice of orthodontics in Westminster, Colorado, from 1984-2006. Upon leaving private practice in 2006, he became a Commissioned Officer in the U.S. Army Reserves, 919th Medical CO (DS) in Aurora, Colorado at the tender young age of 52 as well as joining the faculty at the University of Colorado. He has deployed to Iraq, Afghanistan, and Honduras, and served in the Dominican Republic, Guatemala, and El Salvador.
After teaching for 9 years at the University of Colorado, Dr. Harrell became Program Director of the Orthodontic Residency Program at the Medical University of South Carolina from 2015-2017. In 2017, he relocated to Atlanta, Georgia, to serve as Program Director at the Georgia School of Orthodontics. In the past couple of years, he has lectured at Seton Hill, University of Alabama Birmingham, Medical University of South Carolina, Emory University Oral Surgery Residency Program, Meharry College of Dental Medicine, and Augusta University Oral Surgery Residency Program.
Disclosure: There were no sources of support in the form of grants, equipment, products, or drugs in the production of this article. There are no conflicts of interest, financial or otherwise, in the production of this article.
Click Here to read the original article
